
Reporting for insurers
Business Intelligence with online and interactive reporting
TELUS Health business intelligence tools can provide valuable insights by leveraging a comprehensive database, comprising more than 50% of Canada’s total private health insurance claims. With Business Intelligence you can:

Zone in on relevant data
Retrieve information specific to your customer base, by demographics, drug use, illness or other criteria. With targeted data, you can develop plans catered to your customers.
Identify pain points to refine your service offering
Track trends, from incidences of chronic illness to the impact of aging to manage your plan performance while continuing to meet the evolving needs of your plan sponsors and members.

Build better plans
Inform your strategy with up-to-date information on both historic and current trends. Refine your service offering to optimize program performance.
Here’s what Business Intelligence can do for you
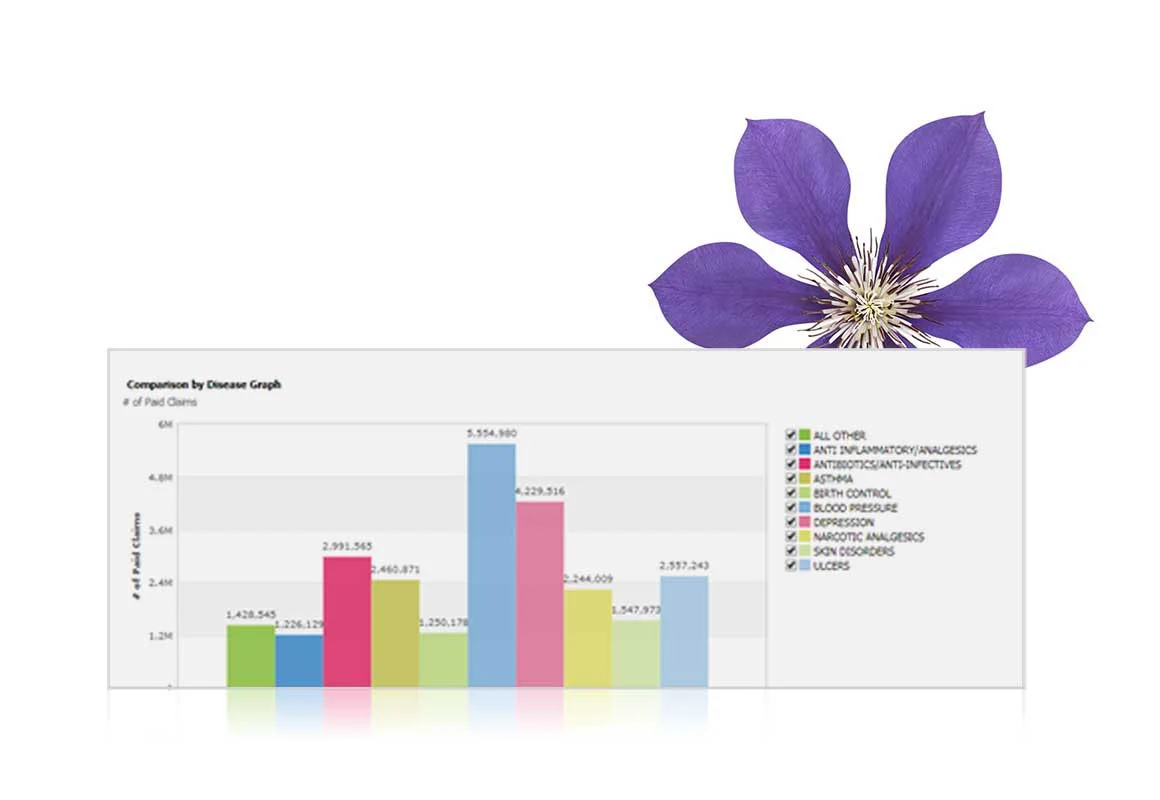
Understand illness and disease prevalence
Identify prevalence of specific illness and chronic disease with robust data on drug use, paired with demographics. With a more profound understanding of member’s health needs, you can refine your drug plan offering.
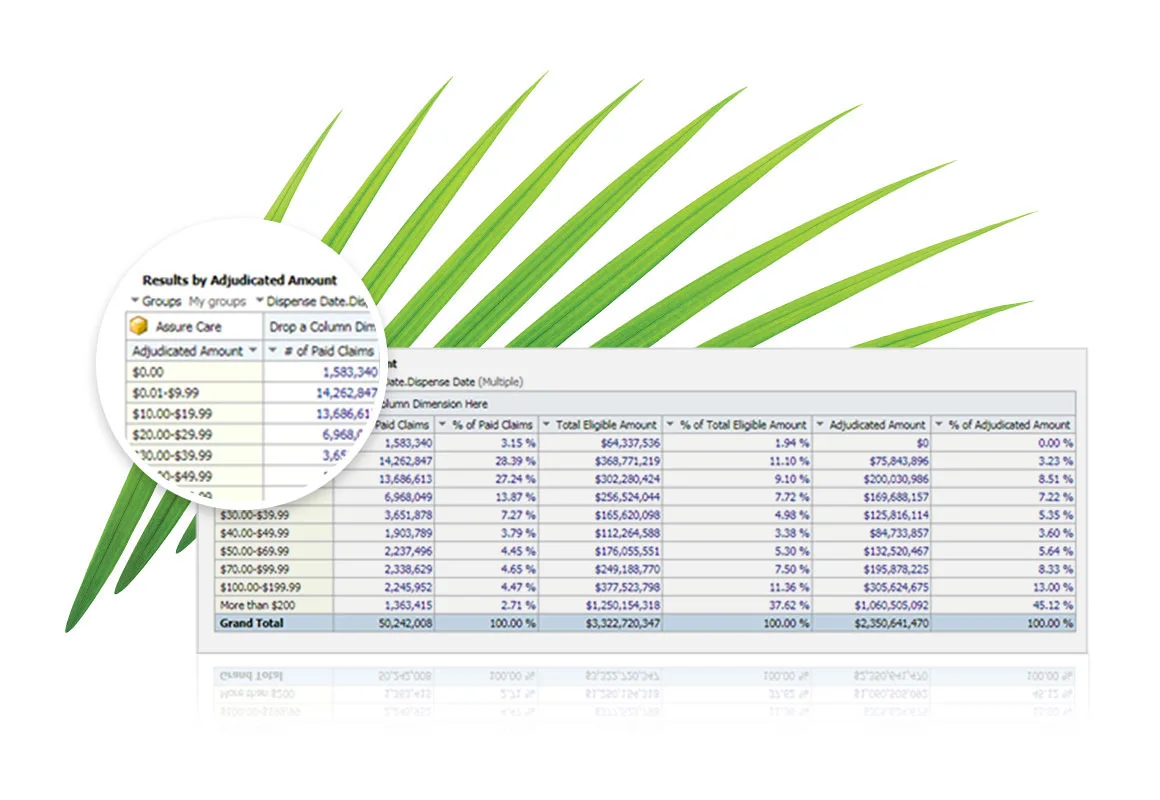
Quantify costs
Filtering data by time frame, age and more, you can better understand the cost of a prescription plan. Refine your strategy based on facts. Know the 50 most frequently claimed DINs, who paid for them, how old they were, and whether it happened in winter or in summer. Refine results based on where you want to optimize your offering.
Protect customer privacy and gather anonymous data
Get valuable insights from de-identified aggregate level data, while still benefiting from a better understanding of the demographic composition driving claims utilization.
More solutions for insurers

My health benefits
Provide plan members with easy access to their benefit plan information and allow them to submit claims via their mobile device or desktop computer.

Claims Exchange
Transmit claims information from the point-of-sale to the TELUS Health adjudication engine and back to the healthcare provider, even if you’re not using a TELUS Health solution.
Request a sales callback
Have any questions or ready to order?
Or call us at:
1 888 709-8759
Monday to Friday: 7:00 AM to 10:00 PM (EST)
Saturday and Sunday: 8:00 AM to 10:00 PM (EST)
Saturday and Sunday: 8:00 AM to 10:00 PM (EST)